How to Improve Physician Well-Being and Reduce Burnout
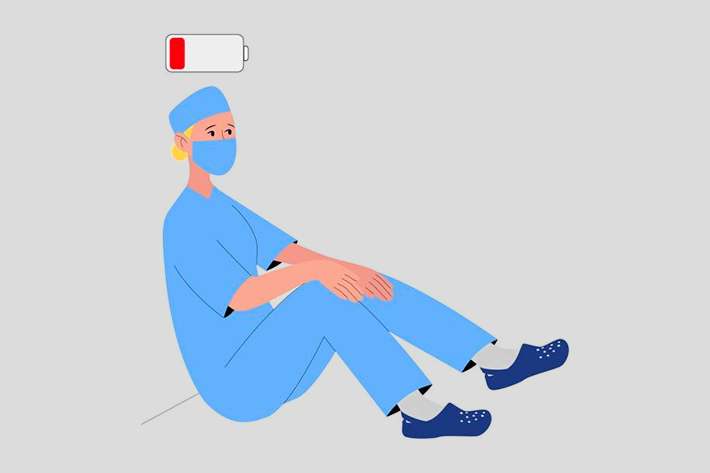

The Challenge
Physicians are experiencing widespread burnout that has only worsened since the pandemic.
Why It Matters
Physician burnout often leads to:
- Higher turnover
- Lower patient satisfaction
- Worse health outcomes


What You Can Do
- Make well-being a top business priority
- Develop & promote resources that address root issues
- Encourage boundary- setting & recognize individuals who set a great example
- Facilitate team bonding
- Emphasize the importance of self- care
Between the long hours, red tape, and often emotionally-taxing work, physicians have long
struggled with burnout. But in the wake of the pandemic, it has only increased in intensity. As you
gear up for another winter season and the COVID wave that will likely come, it’s critical that
physicians feel rested, relaxed, and up to the task.
Quality Reviews CEO Edward Shin, MD recently talked with the physician well-being team at
AdventHealth, including Dr. Leila Durr, Director of Physician Well-Being; Dr. Michael Torres,
Chief Medical Officer; and Mary Dijkstra, Director of Medical Staff Services and Provider
Performance Improvement. Watch the full recording of the webinar above, or read on for
highlights of their conversation below.
What is physician burnout?
Burnout is an occupational phenomenon that occurs as a result of exposure to chronic stressors over time. Signs of burnout include exhaustion, depersonalization, and a decreased sense of accomplishment.
Burnout is especially prevalent among healthcare workers. In a clinical care setting, it may manifest as poor bedside manner, outbursts at work, and cynicism, among other ways.
What causes physician burnout?
There are many different causes of physician burnout, such as:
1. Superhuman expectations
The glorification of overwork and unrealistic demands that physicians experience occur right from the outset in residency, and rarely fade away.
Physicians develop a mentality of “‘I have to be able to solve this. I have to have all of the answers,’” Durr said. “There’s a pressure that they put on themselves — there’s a pressure that society puts on them.”
And in many cases, they even face pressure at home.
“Your neighbors and your family… are all looking to you to be the expert,” Dijkstra pointed out.
2. Compassion fatigue
Compassion fatigue isn’t anything new, but COVID-19 has exacerbated it, “, especially with some of the dynamics and the politicization of vaccination and masks,” Durr explained.
“A lot of physicians are just trying to recommend what’s best for their patients, but they don’t always choose to do that,” she added.
And when physicians must treat those who have become ill as a result of not following the proper protocols, that can be especially frustrating.
3. Systemic obstacles
Another common cause of burnout is moral injury, defined as the distress physicians experience when they are systemically prevented from providing patients with the care that they need.
“Most physicians are going above and beyond to treat their patients to the best of their ability, but then there are all these layers that are telling them, ‘You can’t do this, you can’t do that — you have to jump through this hoop first,’” Durr said. “It’s called death by a thousand cuts for a reason.”
And beyond the systemic factors that impede providers from providing adequate care, there are also systemic societal issues plaguing their most vulnerable patients.
“Physicians are held responsible for 100% of the things that impact health care, and yet we actually only control about 20 percent of that and influence another 30 percent,” Torres said. “I can influence you to potentially cut down on your drinking or cut down on your smoking… but I have no way of impacting what zip code you live in, or whether or not the closest store to you sells healthy food, or whether you can afford an Uber to come to my office.”
What Healthcare Leaders Can Do About Physician Burnout
While burnout is often caused by factors beyond an individual’s control, physicians frequently feel a sense of shame when experiencing it, perceiving it as a personal failure rather than a systemic challenge. This makes it all the more important for healthcare leaders to assist them in addressing burnout — here are a few of the AdventHealth team’s top recommendations.
1. Make well-being a business priority
When Torres started to notice more and more physicians with no history of conduct issues acting out, he knew that something had to be done. Rather than disciplining individuals, though, he began looking into why it was happening.
“We took an approach of wellness rather than punishment,” Torres said. “That’s not to say that we don’t hold people accountable… but we take an approach of ‘What’s going on?’” And the more the team looked into the stressors physicians were facing, the more they realized that their physicians needed additional support. But to do that right, they knew they would need a dedicated program leader.
“There was a recognition that we needed someone at the division level who could actually take this and own it,” Torres said. That led to the creation of the physician wellbeing program in February of 2020, headed up by Dr. Durr.
“It really helps us identify those areas where the physicians are feeling stress,” Djikstra said.
2. Develop & promote resources
After identifying some of the root causes, you’ll need to brainstorm some resources and programs that can help address them. A few of the programs that the AdventHealth team has developed include:
- Therapy
- CME courses
- Wellness classes and workshops
- Massages
- Spiritual counseling
Of course, these programs won’t do much good if people aren’t aware of them, so it’s critical to promote them.
“Dr. Durr sends out a newsletter at least every month that [tells] people where they can go for resources,” Djikstra shared. “We’ve also expanded our communication to office managers and office staff.”
3. Walk the walk
Too many healthcare organizations implementing wellness programs talk about the importance of wellness without actually creating a culture that supports it.
“Make sure that you don’t send mixed messages,” Durr advised. Some organizations, she said, “tell physicians ‘You need to take care of yourself,’ but then double- and triple-book their patients [with appointments] every 15 minutes.”
Encouraging boundary-setting is another important component of a wellness-oriented culture, the AdventHealth team agreed.
“Every one of us has the ability to take on only so much, and setting that boundary… is a very empowering thing,” Torres said. “I encourage physicians to actually draw lines [as] to what they’re willing to and not willing to do.”
If boundary-setting is something your physicians tend to struggle with, you may want to help them do so.
“We’re not going to allow you to be on 15 committees — we’re going to set the boundary for you,” Djikstra said.
One great way to ensure that this culture of wellness flourishes across your organization is by acknowledging those who embody it.
“We’ve actually created a ‘Guardian of Culture’ award for physicians as we build that culture of wellness,” Torres shared. “It’s helpful in planting those seeds here in this organization.”
4. Facilitate teamwork
Physicians are frequently made to feel that they personally shoulder the burden of patient care, but this is a clear recipe for burnout.
“We physicians are taught to be islands unto ourselves. [We’re told] ‘you’re the smartest,’ or ‘you’re the best.’ I heard it on my first day of medical school. But that’s not true,” Torres said.
“Healthcare is a team sport — or at least it should be.”
Torres encourages Physicians to talk with the teams they work with — whether that’s the office staff, nursing staff, or team on the operating room floor — to figure out who owns what, and how they can shift responsibilities if needed.
“As a physician, you are the most highly-educated member of the team, but you are only one member of it,” Torres added. “You will not do nursing as well as a nurse… you will not do respiratory therapy as well as the respiratory therapist.”
Doing this will not only help physicians avoid burnout — it can also lead to better healthcare outcomes.
“Together, the team will be able to carry a lot more weight than just any one individual,” Torres said.
5. Emphasize self-care
As much as physicians tell their patients to take care of themselves, they don’t always follow their own advice. Sometimes, you may need to remind your physicians of how important it is. “One of my big soapboxes that I get on with our physicians is that self-care is part of patient care,” Durr said. “You have to put your oxygen mask on first before you help put it on others.”
Emphasize the importance of good sleep, healthy eating, hydration, exercise, and other self- care practices to your physicians, as well as offering events and programs that provide education and support around these themes.
And make sure that they feel like they can come to you with any other issues — not just to lend a sympathetic ear, but also to assist in addressing the issue. When physicians come to her seeking resources or advice, Durr points them in the direction they need.
“I try to help them figure out where they need to go, who they need to work with [among] the entities and the players in their hospital or in their medical clinics,” Durr said.
Creating Lasting Change
Some factors that cause burnout, like systemic inefficiencies and hurdles, are beyond the control of healthcare leaders. For issues as large as those, healthcare leaders should use their influence to lobby for change — in the meantime, though, they should also take action on what they can control. After all, it’s within their power to create a work environment that supports wellness.
“Burnout is really a signal that something needs to be fixed in the workplace setting or the culture,” Durr said. “It’s like the canary in the coal mine. You don’t blame the canary for not being able to breathe — you figure out what’s going on that you need to fix.”
What is burnout?
Burnout is a work-related phenomenon characterized by exhaustion, depersonalization, and a decreased sense of accomplishment that comes as a result of repeated exposure to stressors over time.
What causes burnout?
Among the factors that lead to burnout are:
- Superhuman expectations: Unrealistic expectations and demands of already busy and stressed physicians.
- Compassion fatigue: Increased sense of apathy or cynicism at work, caused by emotionally-taxing work.
- Systemic obstacles: Hurdles in the healthcare system, as well as societal factors hurting the most vulnerable patients.
What Healthcare Leaders Can Do About Burnout
- Make well-being a business priority: Look into causes of burnout, ideally appointing a dedicated team member to lead the initiative.
- Develop & promote resources: Offer resources and programs that help address the root causes of burnout, such as professional counseling and wellness courses.
- Walk the walk: Create a culture that promotes wellness by practicing what you preach, encouraging boundary-setting, and recognizing individuals who set a great example.
- Facilitate teamwork: Highlight the importance of teamwork, encouraging teams to communicate amongst each other and shift responsibilities if needed.
- Emphasize self-care: Reiterate the importance of practices like good sleep, healthy eating, hydration, and exercise, as well as offering events and programs that support these goals. And when physicians come to you with other issues, help them figure out how to address them.
Creating Lasting Change
Not all of the causes of burnout are within the control of healthcare leaders — systemic issues will require extensive lobbying to change — but those that are within your control can make a significant difference. It’s up to you to create a work environment that fosters well-being and discourages burnout.