5 Things That Drive High Performance in MSSP ACOs
And How Digital Health Tools Can Help You Achieve Them
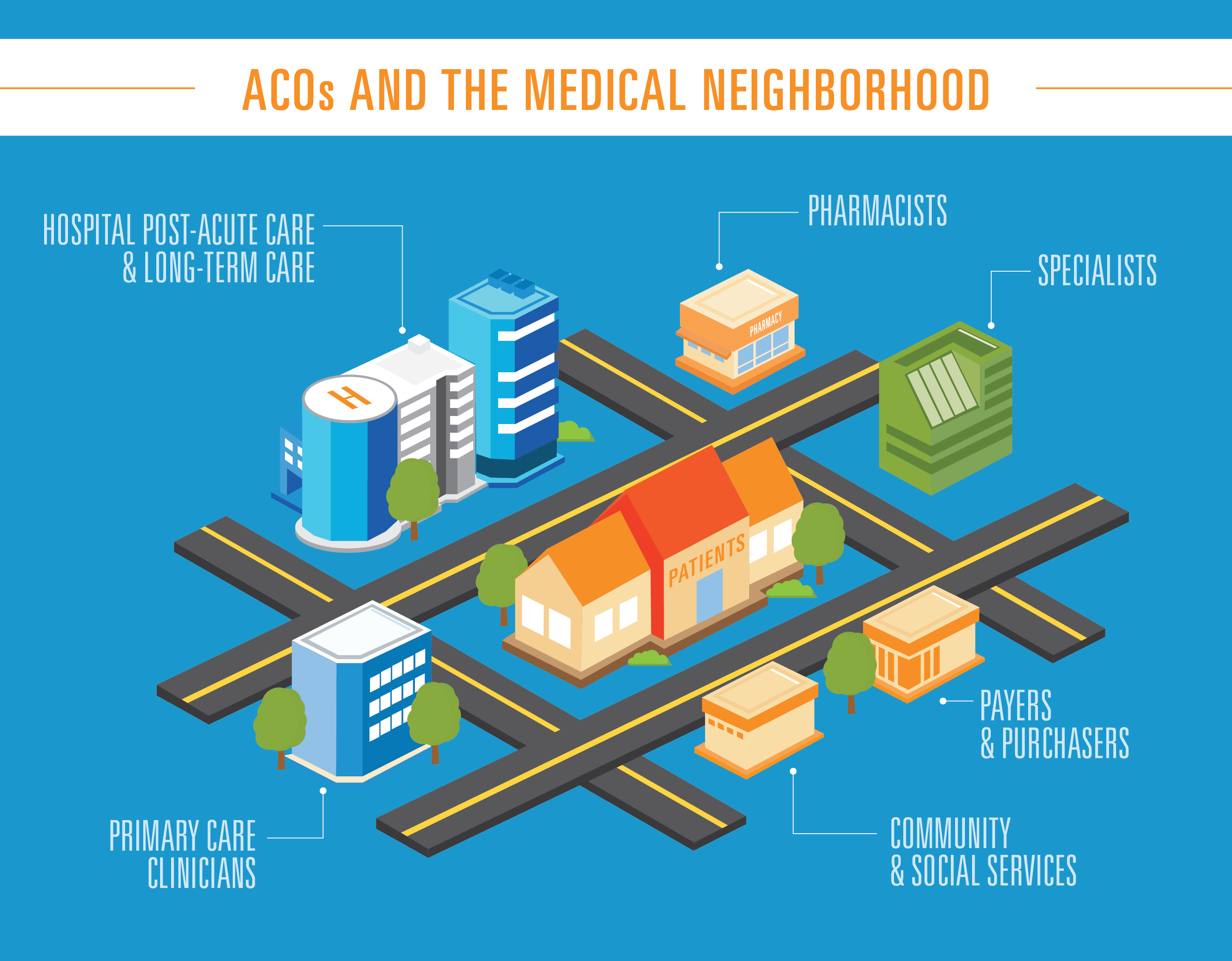
Medicare Shared Savings Program accountable care organizations (MSSP ACOs) are a rare example of a win-win-win. When MSSP ACOs do their job right, members have better health outcomes, Medicare sees savings, and the ACOs themselves get compensated accordingly.
Of course, getting to that point is easier said than done. Each year, hundreds of MSSP ACOs either fail to achieve Medicare savings or even add to its cost. That said, it’s far from an impossible task. In 2022, some 205 MSSP ACOs achieved Medicare savings, which begs the question: What’s their recipe for success?
Unlocking this information isn’t just beneficial for those who fall short of their goals. Even successful MSSP ACOs feel the pressure to improve in the years that follow.
Below, we’ve listed several of the most important strategies that high-performing MSSP ACOs are leveraging to achieve success — and how to replicate their success with the help of digital health tools like Q @ Home.
1. Accurately Capturing Member Risk
High-performing MSSP ACOs understand how important it is to capture all of a member’s different risk factors.
It accurately reflects their patient profile risk, Medicare spending, and comparative benchmarks for their Medicare Beneficiaries, allowing an MSSP ACO to provide the appropriate level of care and spending.
Traditional methods of capturing risk, however, can only help so much. A member’s circumstances can, and often do, change between the initial health risk assessment they must complete upon registration and the government-mandated annual check-ins. And the longer those risks go unaddressed, the greater the chance that they’ll require more serious intervention down the line.
How to Do It
By sending digital health risk assessments in between annual check-ins with a digital tool like Q @ Home, you can capture risks as soon as they appear. And as everyone in healthcare knows, early intervention leads to lower costs and better health outcomes.
Let’s say, for example, that a member’s spouse passes away in March. Their mental health suffers as a result, and they turn to alcohol as a coping mechanism. If you catch that through a quarterly digital health risk assessment in April, you can connect them with the resources they need — like therapy, addiction services, or grief support groups — as soon as possible.
Otherwise, three drinks a day in March could turn to five drinks a day by the time you send the annual health risk assessment in January. Intervening early makes it easier to kick the habit and may even save the member from the damage that 10 months’ worth of heavy drinking can do to their body. And by coding them in April, you can ensure Medicare allows you the additional funds you need for their care in the next year.
2. Pushing Preventive Care Services
An analysis by Care Journey found that the highest-performing MSSP ACOs had higher rates of annual wellness visits and Part B spending. Getting members to attend an annual exam and engage in preventive services like flu shots and colonoscopies does require an initial investment of time and budget. But as the saying goes, an ounce of prevention is worth a pound of cure.
An annual exam today might mean a referral to physical therapy instead of a hip removal surgery in the future. A flu shot today might mean one less inpatient stay in six months. A colonoscopy today might mean a polyp removal versus a partial colectomy and chemotherapy down the line. What’s more, your Medicare Star Ratings for these metrics will improve as well.
How to Do It
Creating a mobile drip campaign with a tool like Q @ Home, a care coordination platform can help you not only remind members of preventive services but also persuade them to engage.
Dynamic content like videos, infographics, and fact sheets combined with a high-response rate channel like SMS text messages makes for a more engaging experience. Creating content that speaks to a variety of motivations/personas, meanwhile, increases efficacy.
Let’s say you have a member, Laura, who’s 65 years old and at high risk for breast cancer. She’s been putting off booking a mammogram — her mother died of breast cancer at 70, and she’s afraid of what they might find. Emails, phone calls, and in-app push notifications have been ineffective.
You add her to a custom campaign you’ve created for patients at high risk for breast cancer. You send a variety of content via text message to ensure that the content gets in front of her. And finally, an infographic on the benefits of catching breast cancer at an early stage assuages her concerns — convincing her to schedule a mammogram.
Related: Boosting Medicare Advantage Acquisition, Engagement, & Retention With Digital Health Solutions
3. Managing Care Transitions
Of course, no matter how much you push preventive services, there will be times when members have to stay in an inpatient facility. Even when the surgery or treatment is a success, however, they’re not necessarily out of the woods.
Each stage in a care transition — whether from a hospital to a skilled nursing facility (SNF) or an SNF to home care — presents an opportunity for information to get lost in translation. High-performing MSSP ACOs understand this and coordinate along the way to ensure that members are getting the care they need. That said, it’s rarely feasible for care coordinators to navigate this manually.
How to Do It
Using a tool like Q @Home allows MSSP ACOs to amplify their efforts to coordinate patient care at scale. Setting up automated workflows for each stage of the care transition ensures that all caregivers are kept in the loop and nothing slips through the cracks — without overwhelming care coordinators.
For example, you can:
- Coordinate SNF care: Send automated wellness surveys to members at SNFs. Scores below a certain threshold & urgent requests are flagged in a dashboard, allowing both care coordinators & SNF staff to follow up & address them
- Improve home care compliance: Send instructional videos, PDFs, etc. Confirm that patients understand/comply with their care plan (e.g. asking them to send a picture of their pillbox or assembled nebulizer)
- Prioritize home health visits: Prompt patients to update you on their status (e.g. asking them to take & record their temperature, send a picture of their wound, etc.) to determine which are most in need of home health visits
All of these actions can help prevent health issues from escalating, avoiding costly and inconvenient readmissions.
4. Monitoring Chronic Conditions
Some members may not require ongoing observation once they exit the acute and post-acute care phases. Someone who has fully recovered after a hip replacement surgery, for example, may be fine as long as they continue to attend periodical appointments. Others, however, may benefit from long-term remote patient monitoring — especially those with chronic conditions.
The most successful MSSP ACOs tend to keep tabs on members with conditions like type 2 diabetes, heart disease, and chronic obstructive pulmonary disease (COPD). This allows them to provide the ongoing support these conditions often require — and ultimately, empower patients to take their health into their own hands.
How to Do It
A tool like Q @Home is useful not just for care transitions, but also ongoing remote patient monitoring. You might want to create a workflow for members with type 2 diabetes, for example. Those who have been recently diagnosed might benefit from receiving educational material and check-ins that ensure they’re following their care plan.
You can also regularly prompt patients to input their weight, glucose levels, and blood pressure. If they start to record worrisome levels, you can flag providers and care coordinators via real-time alerts. In this way, you can reduce the risk of serious adverse health events — and get members the care they need if one does occur.
Related: How Remote Patient Monitoring Can Improve Health Outcomes
5. Ensuring Interoperability
Healthcare too often operates in technological silos. Even physician-based ACOs don’t always use the same electronic health record (EHR) from department to department. So when a member is referred by their primary care provider (PCP) to a specialist, that specialist may not have all of the information they need.
As a result, they often need to reach out manually to the PCP to compare notes — time that could have been spent with other patients. In a worst-case scenario, they may even miss out on critical information that could lead to a misdiagnosis or contraindication.
While MSSP ACOs can’t necessarily control which EHRs their network providers use, they can ensure that the EHR isn’t the only method of communication. The most highly effective MSSP ACOs facilitate interoperability between themselves, their members, and all of those members’ providers to ensure everyone’s on the same page.
How to Do It
A HIPPA-compliant EHR-agnostic platform like Q Reviews provides real-time clinical data to all relevant parties within your preferred provider network. Everyone has access to the same dashboards, even across departments, functions, and in some cases, states.
Having everybody on the same page like this improves visibility, facilitates communication, and keeps the focus on the member. This, in turn, allows you to address their needs faster and better, no matter what their individual care journey involves.
Uplevel Your Operations as an MSSP
Want to learn more about how your MSSP can reach peak performance? At Q Reviews, we have more than 10 years of experience helping healthcare organizations better understand and serve their patients and members. Request a demo or reach out to us to learn how our suite of digital health solutions can help you acquire, engage, and retain members.