Nurse Burnout & Moral Injury: Addressing the Current Crisis
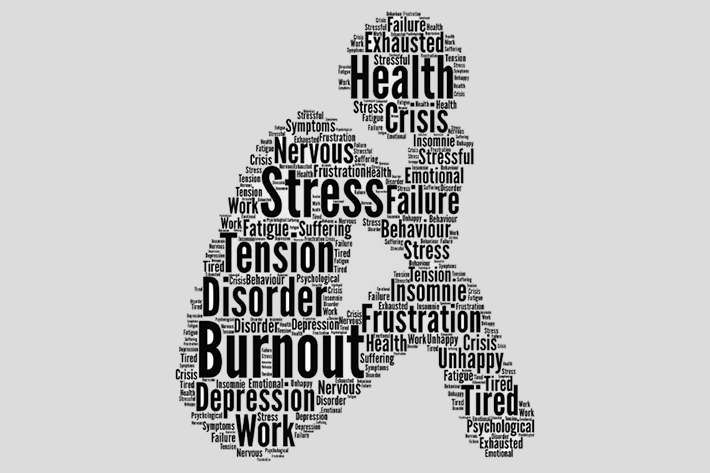

The Challenge
Nurses are experiencing widespread burnout that has only worsened since the pandemic.
Why It Matters
Nurse burnout is often associated with:
- Higher turnover
- Lower patient satisfaction
- Worse health outcomes


What You Can Do
- Solicit feedback from the frontline & act on it
- Offer a respite room & encourage staff to take breaks
- Foster unity through buddy/mentorship programs or team bonding events
Nursing is an intrinsically demanding field: the hours, pressure, and expectations that come with the job have always lent themselves to burnout. But in recent years, burnout has reached crisis-level proportions. A survey of 2,500 nurses released in July 2022 found that three-quarters of respondents had experienced burnout since the pandemic began, and 64% were considering leaving healthcare altogether. In the midst of already widespread nursing shortages, identifying the causes of burnout — such as moral injury — and addressing them is critical to improving patient care.
This was the focus of a recent webinar hosted by Quality Reviews CEO Edward Shin, MD. In it, he spoke with the team from Resilient Seven — a coaching platform that aims to teach practitioners how to combat burnout and moral injury — all of whom have worked as nurses themselves.
Read on to learn what Founder and President Vicky Reiser, Director Of Operations Joe Zimmerman, and Vice President and Director of Strategy Léa Martineau have to say about identifying and preventing nurse burnout and moral injury.
Nurse Burnout on the Rise: Is Moral Injury to Blame?
Conversations around nurse burnout often center around staffing shortages. And while that does play a role, there’s more to it than just that, the Resilient Seven team agreed. A few of the most pervasive factors include:
- Alarm fatigue: With technology making us more available than ever, nurses must deal with a deluge of requests at any given moment.
- Information overload: In addition to caring for patients, nurses are expected to keep up with all of the latest information in the EHR, physical paperwork, research journals, and more.
- Compassion fatigue: Day after day of emotionally taxing work can leave nurses feeling emotionally exhausted.
- Profit-margin crunches: Because healthcare costs are skyrocketing, nurses are constantly under pressure to do more in less time.
- Systemic disconnects: Nurses often find themselves torn between their own duty to care for patients and the expectations that their employers, industry regulators, and payers place on them.
- Moral injury: Systemic bureaucratic hurdles often prevent healthcare personnel from being able to provide the best patient care that they can.
The 7 Practices That Build Resilience in Nurses
Reiser experienced many of these issues in her first nursing job in oncology at 22, eventually leading to a period of moral injury and burnout. She later enrolled in a graduate program, where she began to study burnout, what causes it, and how to combat it.
In the research she did for her projects and talks, she subsequently noticed seven frequently recurring themes that helped improve nurse resilience:
- Awareness: Understanding yourself and recognizing your thoughts and feelings
- Mindfulness: Practices that keep you grounded in the present
- Gratitude: Reframing negative experiences to appreciate what you’ve learned from them
- Self-care: Practices that improve your overall well-being, like rest, nutrition, exercise, sleep, and time off
- Meaningful relationships: Working to concurrently improve relationships with friends, family, patients, colleagues, and leaders
- Moral courage: Learning how to stand up for what’s right and cope when your ethics have been tested through moral injury
- Purpose: Focusing on what drives you, not only as a nurse but also as a person
Eventually, she was introduced to a company whose platform allowed her to build an interactive educational program based on these seven core principles: Resilient Seven. Three times a week — at a time chosen by them — users receive a link via SMS to a 90-second to two-minute educational module incorporating videos, quizzes, and short responses, all based on the seven components of resilience.
“We’re able to dive down into these seven concepts to quantify how well someone’s doing… we have free response questions as well that enable us to feedback information that the user is providing,” Reiser said. “It’s a coaching program for the frontline user, but also an advocacy tool and engagement tool for leadership.”
What Healthcare Leaders Can Do to Combat Burnout & Moral Injury
Between being nurses on the frontline themselves and then developing a program designed to
counter burnout, the Resilient Seven team had a number of suggestions for what healthcare
leaders can do to fight nurse burnout in their own organizations.
1. Engage your team
As well-intentioned as they might be, pizza parties probably aren’t going to address the issues
at the core of burnout in your organization. And the only way to figure out what will is by hearing
from your frontline staff directly. Martineau recommended implementing employee engagement
surveys, making sure to emphasize that you want to hear what they really think — not just what
they think you want to hear.
“I always encourage my staff to be authentic and genuine in their responses, even if they think
it’s not going to make me happy — I need to get the real pulse on the organization,” Martineau
said.
And of course, once you get that feedback, you need to act on it. One thing you may want to
consider in particular is changing up your incentives.
“I spent a week in Washington taking classes on healthcare, and my big takeaway was that
incentives are completely misaligned,” Martineau shared.
She recommended healthcare leaders decide what they want to prioritize, and think about which
incentives may help them reach those goals.
“[Nurses] might want more money, but are there other things? Do they get to recuperate without disruption when they’re not on their shift?” she said. “I think that we have to look into incentives
broadly across the board.”
To hold yourself accountable, Martineau recommended including a question like “Do you feel
like we addressed the results from the last survey?” to any future surveys.
2. Offer & encourage breaks
Offering nursing staff a dedicated space like a respite room where they can unwind — if even
for a moment — can give them a much-needed opportunity to collect themselves and recharge.
But too often, Reiser said, nurses are hesitant to take advantage of them.
There’s a respite room on the inpatient floor she works on, but “people feel guilty about using it,
or they feel bad [asking a colleague], ‘Hey, can you take my phone while I go sit in the respite
room for 10 to 15 minutes?’” Reiser shared. “There’s this unfortunate culture in medicine and
healthcare of martyrdom — that I can’t leave my position.”
She recommended emphasizing the importance of self-care, not just for nurses’ own well-being,
but for their patients’ too.
“That’s something that we talk about routinely in the Resilient Seven curriculum… you are
always better if you take care of yourself,” Reiser said. “Spending five minutes away from the
bedside is honestly going to make you a more productive and clear-headed individual.”
There may be some staff that are still skeptical, but Reiser had a novel suggestion for what to
do in that case.
“If you have staff that are reluctant, you can say, ‘Okay, let’s do a mini study. Tell us how you
felt and how productive you were during this shift where you didn’t take any breaks at all. Then
take a day where you have maybe two five-minute stints where you sit in that respite room and
tell us how you felt and how productive you were after that.’”
3. Foster unity
The Resilient Seven team agreed that no matter how challenging their jobs have been, the thing
that has always gotten them through is their colleagues.
“Early on in the pandemic, we saw this great surge of [nurses] banding together,” Zimmerman
said. “We really didn’t have the workforce at that time. But we came together and we made sure
that we supported each other” — allowing them to do far more than anyone could have
expected.
“My biggest recommendation is [to] build those meaningful relationships with who you’re
working with,” Reiser agreed. “That was what helped us survive those difficult days.”
To help those relationships flourish, you may consider implementing a buddy or mentorship
program — as Reiser did earlier in her career — or offer team bonding events.
A Better Future Is Possible
There are a number of complex factors contributing to nurse burnout, none of which are easily
fixed — but the Resilient Seven team fully believes that things don’t have to stay the way they
are.
“I understand the cynicism that people might experience at this time, but I feel very hopeful.
There are tools, there’s some traction, there are people that want to make a difference,”
Martineau said. “I have great hope that we’ll get to a better place — that we’ll rally and improve
how we care for ourselves as well as our patients in the next couple of years.”
Causes of Nurse Burnout
Among the factors that lead to nurse burnout are:
- Alarm fatigue: The constant stream of requests and alerts that come in
- Information overload: The overwhelming volume of data nurses must read and record
- Compassion fatigue: Exhaustion caused by emotionally taxing work
- Profit-margin crunches: Being pressured to do more in less time due to skyrocketing health costs
- Systemic disconnects: Practitioners, employers, industry regulators, and payers all have different goals and priorities
The 7 Practices That Build Resilience in Nurses
- Awareness: Understanding yourself while recognizing your thoughts and feelings
- Mindfulness: Practices that keep you grounded in the present
- Gratitude: Reframing negative experiences in order to appreciate what you’ve learned from them
- Self-care: Practices that improve your overall well-being, like rest, nutrition, exercise, sleep, and time off
- Meaningful relationships: Working to improve relationships with friends, family, patients, colleagues, and leaders concurrently
- Moral courage: Learning how to stand up for what’s right and cope when your ethics have been tested
- Purpose: Focusing on what drives you, not only as a nurse but also as a persNurseon
What Healthcare Leaders Can Do to Help
- Engage your team: Survey employees so that you can find out what they really want and need. Then, act on it and hold yourself accountable for change.
- Offer & encourage breaks: Create a respite room if you don’t have one already, and encourage staff to use it — remind them that self-care is patient care.
- Foster unity: Consider implementing mentorship programs or hosting team bonding events to build community and improve support among your staff.
A Better Future Is Possible
There are a number of complex factors contributing to nurse burnout, none of which are easily
fixed — but with the tools, traction, and people needed to make it possible, they can be
overcome.