Social Determinants of Health (SDoH): Not Just a Buzzword

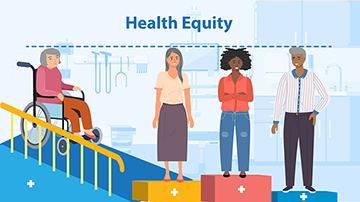
Social determinants of health (SDoH) are finally getting the attention they deserve in the healthcare industry — many organizations are making major investments to account for them. Effective healthcare population management, of course, means identifying health disparities, learning how they impact care delivery, and coming up with solutions to improve healthcare outcomes while reducing healthcare costs.
One of the largest investments into SDoH has come from the Center for Medicare & Medicaid Services (CMS). Their landmark CMS Framework for Health Equity report aims to address health disparities in every community across the country. Using five priority areas, CMS will use this framework to design, implement, and improve SDoH policies and programs. Specifically, they aim to provide indigent and underserved populations with the care and support they need.
Already, 57 health systems across the country have spent $2.5B on SDoH, health equity, and healthcare population management programs. These investments focus on improving healthcare outcomes through employment, education, food security, social community, and transportation, among other factors.
The ACO Reach model, for example, offers a new payment approach to better support care delivery and coordination for underserved patients. The program will require all participants to develop robust health equity plans to reduce health disparities within their patient populations.
It’s no surprise, then, that SDoH has become a hot topic among digital health companies, healthcare thought leaders, and conferences. There’s no doubt that the call to shift our mindset and care strategies to include SDoH is growing. However, many in the industry have been slow to take action, citing financial challenges.
But the truth is, investing in social determinants of health can reduce healthcare costs and improve healthcare outcomes. Below, we’ll explain how.
SDoH & Healthcare Costs
Providers and payers have always struggled to balance financial health with quality care. And in the wake of the pandemic, when so many healthcare organizations suffered losses, this has become even more urgent. Organizations struggling to stay afloat after revenue loss from COVID-19 have made managing overall healthcare costs a top priority. But you don’t have to choose between low costs and great care — addressing SDoH can directly reduce the average cost per patient.
In June 2021, a Journal of the American Medical Association article linked SDoH with higher Medicare spending per beneficiary. After looking at spending data for over 3,000 counties caring for 33 million Medicare FFS beneficiaries, the study found that those with the highest Medicare spending also had a higher rate of SDOH challenges. These counties also saw health disparities like more cases of chronic illness and cancer — two major drivers of costs.
Preventative measures can directly reduce the risk that leads to higher healthcare costs, however. This makes it critical to promote access to primary care, health literacy, wellness programs, and community care coordination.
SDoH Barriers & Readmissions
Between the hospital readmission penalty and the cost of additional care, readmissions and emergency visits can significantly increase costs. With advancements in care reducing certain types of readmissions and emergency visits, SDoH and health equity challenges are now among the highest drivers. By addressing SDoH and focusing on healthcare population management, health systems can reduce readmissions by up to 20%.
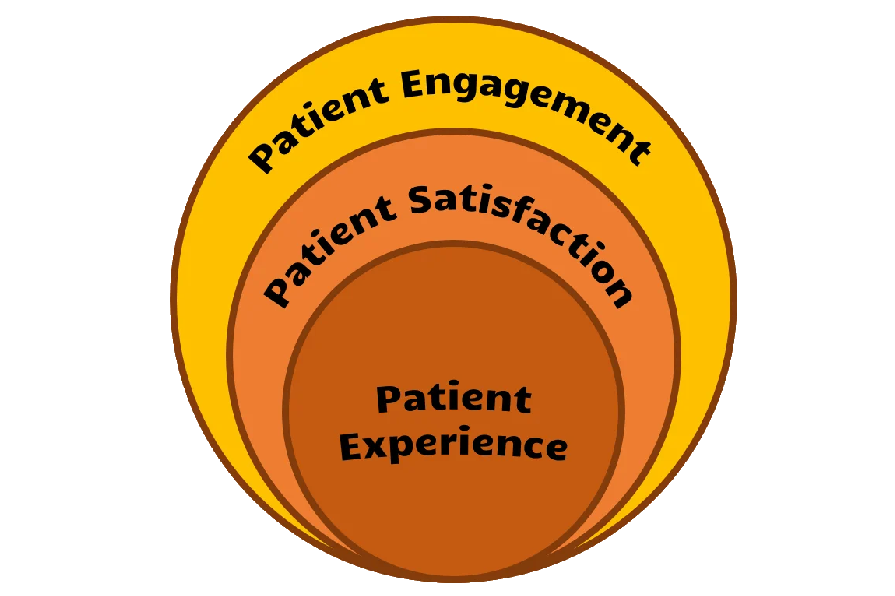
One way to do this? Gather and act on feedback not just at the care site, but across the entire care journey. This allows providers and payers to identify and overcome SDoH challenges before they lead to a readmission. But gathering meaningful feedback means going beyond simple ratings and “yes/no” questions. You must ask the right questions and feed this data into risk prioritization calculations.
Health Access & No-Show Appointments
No-shows and limited impact the bottom line in both the short term and the long term. What’s more, patient health may worsen when necessary appointments are missed, leading to a higher overall cost per patient.
Assessing a population’s unique, local social determinants of health and health equity challenges can introduce several preventative measures and interventions that can be integrated into healthcare organizations’ access strategy. Many of the issues linked to no-shows are tied to:
- Housing
- Transportation
- Social Support
- Education
- Economic Stability
- Community and Neighborhood Environment
Providers and payers need to increase the number of channels of engagement that address each of the unique SDoH challenges that impact their patient segments.
Value-Based Care Agreements
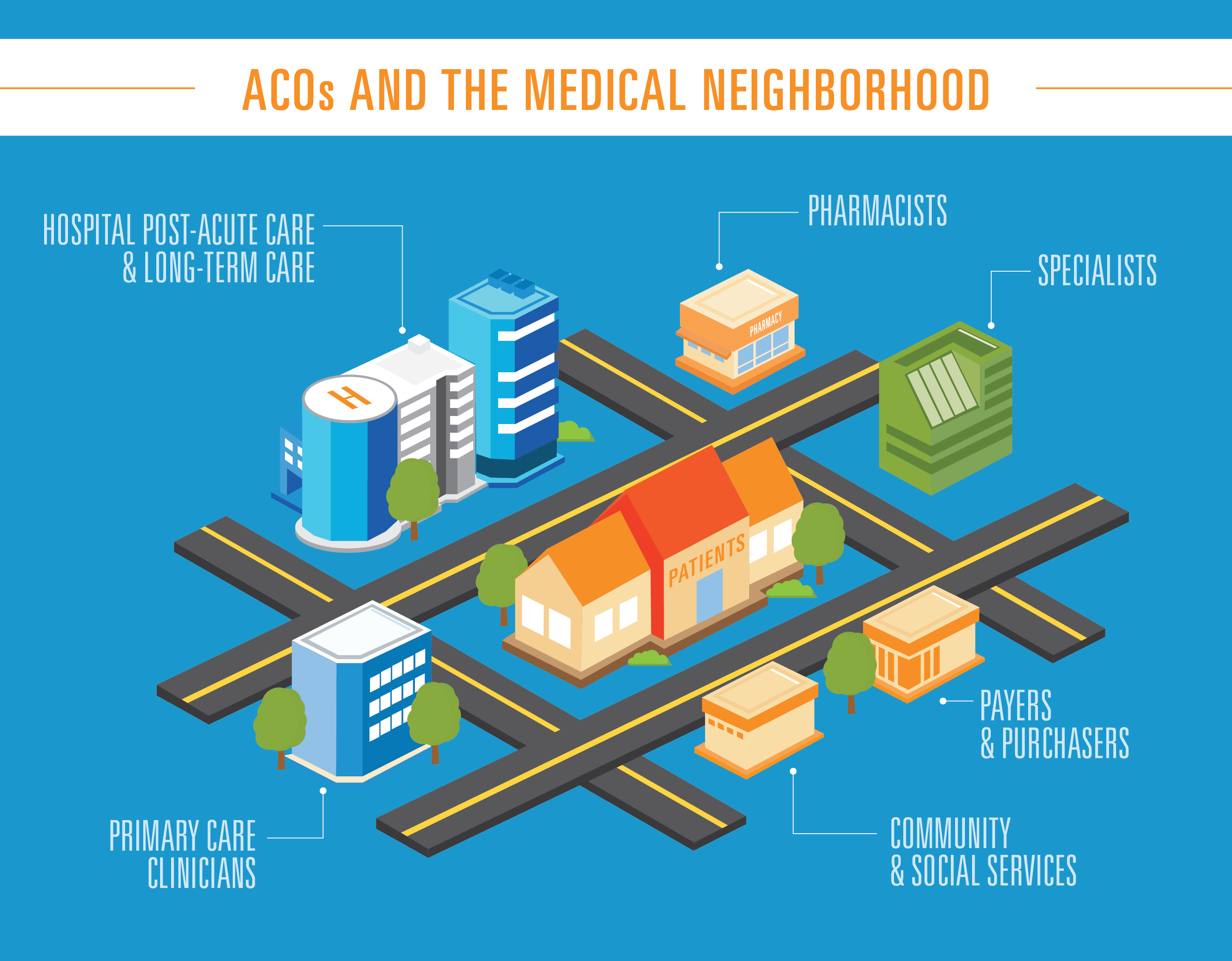
Value-based care is on the rise. Whether it is managing bundle payments or full capitated risk, value-based care agreements marry financial and clinical healthcare outcomes. The key challenge within these agreements is the difficulty of micromanaging a patient or member’s care. This becomes all the more tricky when SDoH are involved.
MSSP ACOs, Medicare Advantage, and ACO REACH participants need to manage patients across different care settings and ensure care pathway adherence across the continuum. Elements of care pathway adherence impacted by SDoH and health equity can include but are not limited to:
- Medication adherence
- Therapy
- Dietary plans
- Follow-up appointments
- Wellness checks
Organizations can focus on empowering care navigation and care coordination teams by developing community health networks and integrating SDoH and health equity assessment tools in their Transitions of Care guidelines