Healthcare Innovation: How New York-Presbyterian Approached Patient Experience During the Pandemic

Healthcare providers worldwide are no strangers to catastrophic events: the AIDS epidemic, SARS, the Ebola outbreak, and more. Adapting to these crises required major healthcare innovation. However, the pandemic is nothing like we’ve ever seen in our lifetimes. It’s pushing front-line workers to adjust their plans hour by hour while also trying to keep the patient experience in mind.
With circumstances quickly changing, hospitals must be ready to move forward at any given moment. No amount of schooling could have prepared front-line workers for COVID-19’s devastation.
In our webinar, “New York-Presbyterian’s COVID Experience,” Quality Reviews® CEO Edward Shin, MD, has an engaging conversation with Rick Evans, Chief Experience Officer for New York-Presbyterian Hospital, about using healthcare innovation to address the needs of both patients and staff during the pandemic.
Staying Ahead of the Worst-Case Scenario
Evans knows the struggle of responding to crises all too well. He witnessed the aftermath of 9/11 and the Boston Marathon bombings. Still, responding to the pandemic is a completely unfamiliar experience, even for an experienced professional such as himself.
“COVID is like nothing else I’ve seen. It was terrifying. I had chills up my spine almost every day,” he recalled.
Luckily, New York-Presbyterian had more resources that many other hospitals weren’t fortunate enough to have. The staff never ran out of PPE, and they made sure they were always 12 hours ahead of anything that might come their way.
“We are as ready as we can be for any surge,” he said confidently.
Evans knows that true healthcare innovation is about more than just having masks and face shields at the ready. He built a solid plan to help out employees and collect patient satisfaction data so the organization always knows what’s going well and how they can improve.
Creating a Safe Space for Employees
At the height of the pandemic, the workers at his hospital especially struggled with the fact that they were caring for a high volume of patients while being highly susceptible to contracting the virus themselves.
“This is a different moment that requires a different approach for the front line,” Evans pointed out.
He recalled the healthcare innovation programs he put in place at New York-Presbyterian to prioritize employees’ mental and physical health.
“People were afraid to go home after work. There were lots of empty hotel rooms in New York, so we [reserved] them,” Evans shared.
The hospital provides other types of support — such as food, elder care, and childcare — for its employees to keep them healthy and reduce stress.
For front-line healthcare employees, fear, anxiety, and depression are prevalent — both openly and privately. Evans knows that some are afraid to put themselves out there and talk about their struggles. This is a product of what he calls the “suck-it-up” culture. His response was to offer bereavement counseling, prayer circles, and spiritual support.
Evans knows all too well the effect of hospital work on a person’s mental wellness. His friend and colleague, Dr. Lorna Breen, suffered from depression and died by suicide after she got COVID-19.
“She didn’t bounce back, physically or psychologically,” Evans said.
That tragic experience encouraged him to expand his employee care strategy.
“You have to go to people and talk with them. Put resources in their face. Make it okay for people not to feel good and to have a space where they can say, ‘I’m not in a good place,’” Evans advised.
Making a Difference Through Leadership & Healthcare Innovation
Evans also gets insight into how people are doing by opening up to them.
“I found as a leader, the most important thing I can do is be transparent about my own feelings,” Evans shared.
Now, he asks how his employees are doing at every meeting to bring conversations about mental well-being out of the shadows.
“When you normalize [talking about your emotions], you neutralize the ‘suck-it-up’ culture a little bit,” he explained.
Evans urged other healthcare organizations to check on their teams on a regular basis.
“We need to take care of each other through this. We need to go beyond the niceties and really have to watch and care for each other in a much more intense way,” Evans said.
At Quality Reviews®, we’re leading the way in healthcare innovation through technology. Our Q-Employee lets healthcare organizations find out how healthcare workers are doing by sending out employee satisfaction surveys. If people don’t feel comfortable sharing in an open setting, it can help you find out what they need to get through this tough time. Better employee wellness translates to a better experience for patients, too.
Starting and continuing the conversation about emotional health helps reduce burnout and risk in healthcare systems. This also plays a key role in enhancing the patient experience.
Keeping Lines of Communication Open with Patients
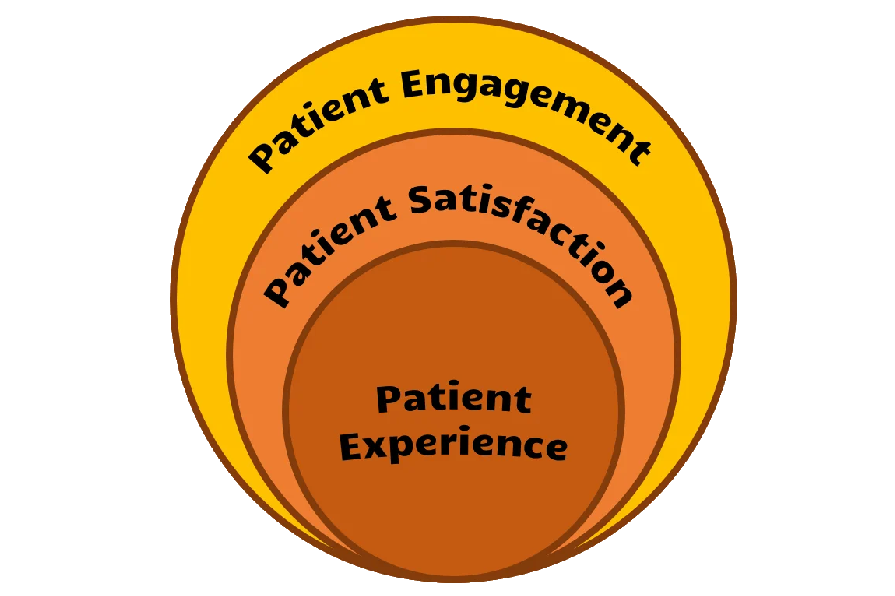
Creating world-class care requires supporting patients at every step of the process.
“The heart of it is communication,“ Evans said.
New York-Presbyterian’s communication strategy includes using Q-Reviews® to send patient surveys via text so they can get real-time feedback on how things are going. These evaluations only have 5-8 questions to make sure they’re easy and fast; that improves completion rates. According to Evans, paper surveys are no longer feasible, reliable, or relevant in today’s healthcare landscape.
Q-Reviews® automatically sends different patient experience survey questions based on the department and type of care the patient received so that each question is personalized, providing better data. Plus, it allows for speedy service recovery so you can fix what’s gone wrong faster than if you were processing paper surveys.
Evans’ philosophy of communicating openly also extends to potential patients. He said, “We should be able to make [patient satisfaction survey results] available to the public so we can help consumers make [their own] decisions.”
Q Reach provides healthcare organizations with the ability to post provider reviews on their site to build trust with prospective patients. 84% of respondents from the 2019 Local Consumer Report Survey said they trust online reviews just as much as they would personal recommendations.
Evans believes there’s a need to improve transparency in healthcare: “Let’s evolve, make the data available, and [become] more nimble than we are today.”
Getting all employees on the same page is a big part of enhancing the patient experience program. New York-Presbyterian improves care by having front-line workers and patient advocates work together to make patients’ time at the hospital a truly healing space. With everyone aligned and collaborating to build better patient-provider communication, the staff works in lock-step and drives a better NPS.
What’s Next for Patient Care?
COVID-19 has shed some light on pressing issues in the healthcare industry as a whole.
“COVID showed there are a lot of things in healthcare that need to change,” Evans explained.
The silver lining for the healthcare system is that COVID-19 brings up a meaningful conversation on how healthcare organizations can learn from their COVID-19 response strategy to make everything more efficient post-pandemic.
In the past, healthcare had many bottlenecks that stood in the way of a positive patient experience.
“We can move fast if we need to,” Evans said. “If we can change ICU beds overnight, why are we so slow [in other areas]?”
As a result of the pandemic, many experts predict giant shifts in healthcare. However, there are still many open questions: How will the waiting room experience change? Will people move through the check-in more quickly to get care faster? When will using pen and paper for patient intake forms become a distant memory? What role will telemedicine play after COVID-19 is long gone?
We’re starting to see some organizations adopt advances in healthcare innovation, but it’s difficult to say what’s next for the industry as a whole.
Preparing for the Post-Pandemic Future
No matter what the next trends are, COVID-19 has forced healthcare workers to overhaul their old patient care methods.
During the webinar, Evans gave valuable, real-world insight into how the patient experience is more than checking in on someone frequently or having a considerate bedside manner. It’s about looking at all factors that could affect the patient and taking action to make it better. Whether that’s creating an air-tight plan for the next surge, asking your employees what support they need, or responding within minutes of receiving feedback, you can create an outstanding patient experience more easily and efficiently.
Want to watch the full webinar? Head over to this page to catch the whole conversation.
Interested in learning more about how Quality Reviews® can help you improve your patient experience and net promoter score? Let’s talk. Contact us to learn more about our solutions or schedule a demo.