How to Streamline Patient Throughput

From intake to discharge, there are a number of different challenges that can emerge and slow down throughput in healthcare. And inefficient throughput isn’t just a problem in itself. Often, it leads to compounding challenges.
Patients who have to wait on their providers for long periods of time are less satisfied and less likely to return to your organization — they may even recommend that friends and family members stay away. Staff are likely to be frustrated by inefficient throughput as well, which can lead to disengagement and even turnover. Combine this with longer lengths of stay and higher inpatient costs, and it all converges in significant financial issues for healthcare organizations.
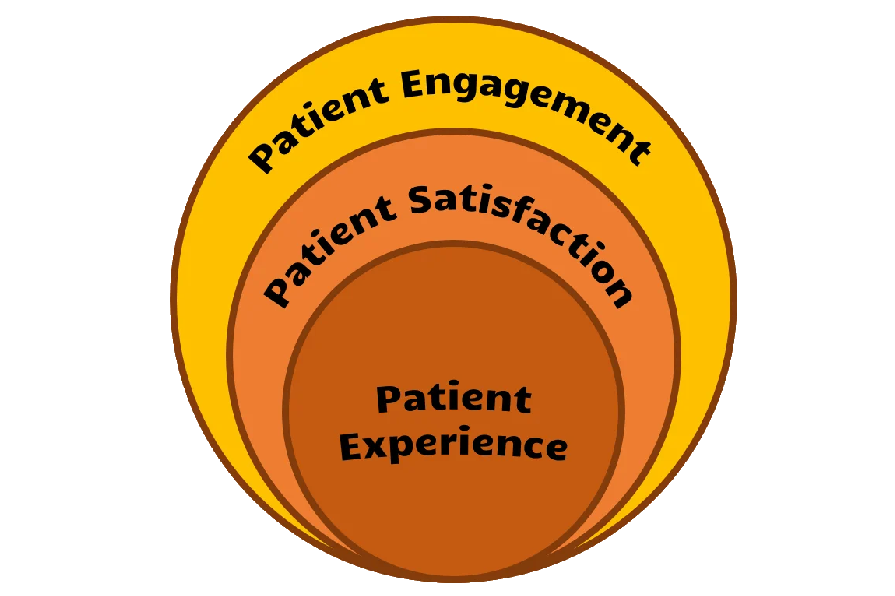
For health organizations, the takeaway is clear: improving patient throughput is critical. While it might seem daunting to change established processes, improvements to throughput in healthcare can help with improving patient experience scores, boosting patient retention rates, reducing hospital length of stay, and ultimately, increasing revenue.
And with the help of digital tools, making improvements to your throughput can be easier than you might think. Below, we’ve listed a few ideas for using digital tools to address and overcome common obstacles in patient throughput — read on to learn more.
Throughput Challenges From 3 Perspectives
Before jumping into the solutions themselves, let’s set the stage by looking at throughput challenges from the perspectives of the three main groups of stakeholders: patients, staff, and health systems.
Patients
In inpatient settings, the chief complaint from patients is nearly always lengthy wait times. Beyond waiting for doctors or nurses to make their rounds so they can discuss their diagnosis or ask them questions about their treatment, patients often must wait for long stretches of time for requests as simple as a blanket for a cold room. And when patients have no visibility into when they can expect to see staff or when their requests will be addressed, it’s even more frustrating.
Staff
Over the years, clinical staff have seen their responsibilities greatly increase while still having to attend to the same number of patients. In addition to actually providing care, many clinical staff have to spend two hours a day or more knee-deep in EHR systems doing administrative work. After the COVID-19 pandemic brought an influx of patients and spurred mass resignations, nurses, physicians, and other clinical staff have become even more overwhelmed. When clinical staff are as bogged down as that, staying on top of individual patient requests and managing tasks for efficient throughput in healthcare becomes all the more difficult.
Health Systems
Many health systems today are financially strapped. As fewer staff leads to longer hospital stays, the cost of providing inpatient services is increasing while reimbursement decreases. So even as volume accelerates, revenue doesn’t necessarily keep pace. On top of that, health systems are struggling to hire as many clinical staff as they need, which makes it harder to give patients the level of individual attention that they need and meet their requests. Operational challenges like these only compound costs, creating a cycle in which lower revenue makes it even more difficult to hire staff.
Digital Solutions to Improve Throughput in Healthcare
So, which digital tools can help address patient throughput challenges like the ones listed above? We’ve listed several ideas below, bucketed into a few different categories.
Feedback
All patients want to feel like their voice is being heard. Without an adequate feedback platform, though, it’s difficult for them to feel that way. Providing an easy way for them to give feedback — like via text messaging — allows patients to advocate for themselves and helps clinical staff proactively improve patients’ stays. Rounding tools, meanwhile, can help consolidate patient requests and flag urgent ones that require immediate attention.
Lean More: Q Visit — Listen in Real-Time While Patients Are in Your Care
Education
A big part of improving patient satisfaction is simply setting expectations. When patients don’t know what exactly their stay will involve, they can feel blindsided and even upset that things haven’t gone the way they had envisioned. Consider sending educational material via text message — like videos, visual-forward PDFs, and checklists — that explains patients’ treatment, provides them with instructions, and addresses frequently asked questions.
Once a patient actually checks in, you can continue to send them resources that explain instructions and next steps to proactively prepare them for discharge. The more you educate your patients, the more they’ll comply with instructions — which can lead to shorter stays and better health outcomes.
On the staff’s end, consider replacing patient dry-erase whiteboards with digital whiteboards that contain real-time nursing and medical information. That way, a quick glance will allow clinical staff to get up to speed without having to rely on outdated information or decipher sloppy or partially-erased handwriting. What’s more, staff won’t have to go through the redundant process of transcribing all of the information they already entered into the EHR onto a whiteboard.
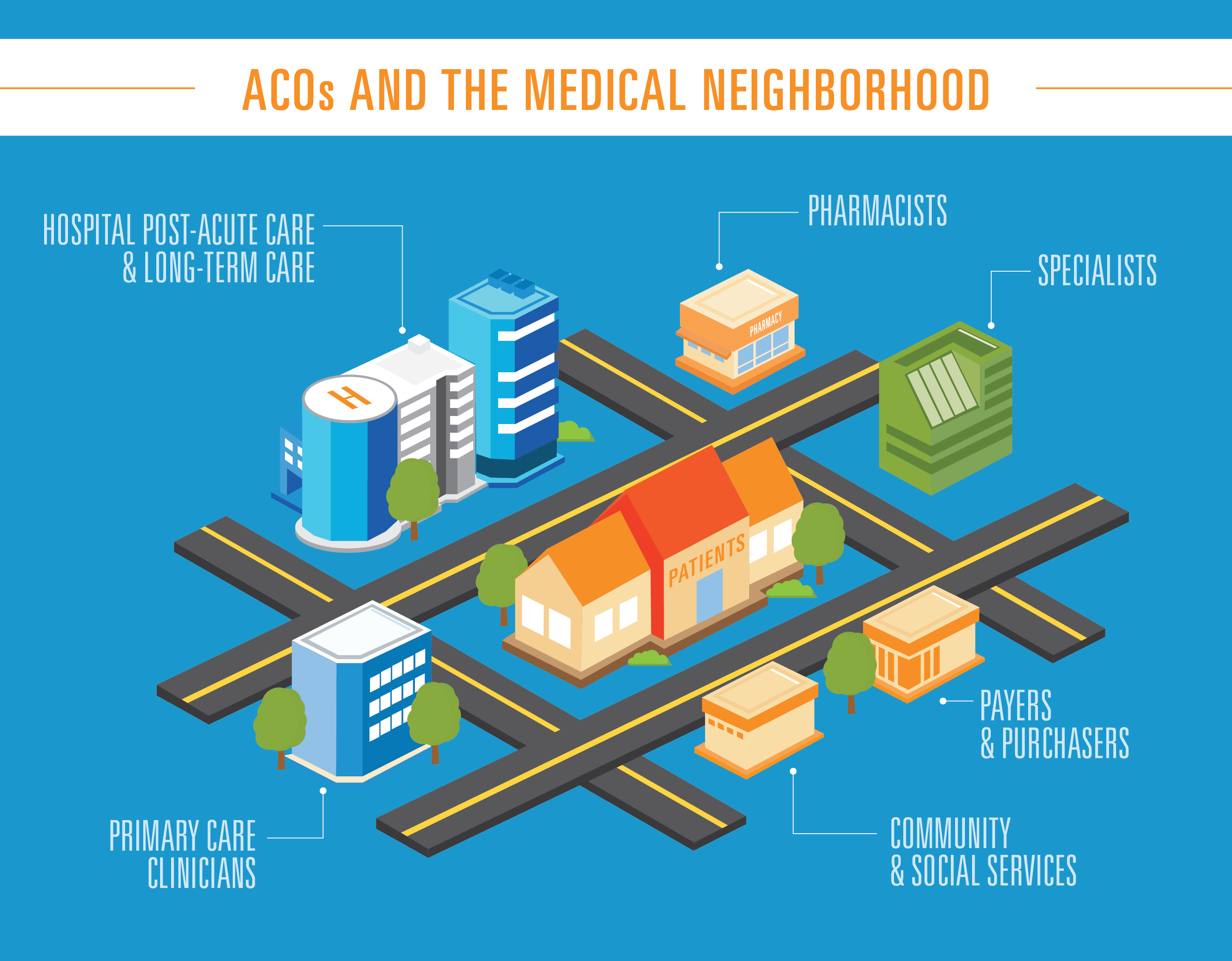
Operations
At most hospitals, patient requests will be shared en masse with a patient’s entire care team, even if they’re not the ones who can address them. Look into a platform that not only aggregates patient requests, but offers smart tasking routing that directs requests to the appropriate contacts. A request to raise the temperature of a patient’s room, for example, can be directed right toward the facilities team rather than requiring care staff to manually contact them.
And as patients wait for requests to be fulfilled or see a member of their care team, sharing wait-time notifications and status updates can reassure them that their concerns are being actively addressed. Some delays are unavoidable, but if a patient knows when they can expect a resolution, they become a lot more tolerable.
One stage where wait time can be easily reduced, however, is discharge. Sharing discharge forms and instructions over text can initiate discharge planning earlier in a patient’s stay.
Sharing information around items like medications and at-home care earlier on allows patients to discuss them in detail with their provider, improving comprehension of their treatment plans and post-discharge success. It also prevents patients from being overwhelmed by a deluge of paperwork at the very end, which can reduce the anxiety associated with discharge and speed up the process.
Start Streamlining Your Patient Throughput Today
Patient throughput is a complex process composed of many different moving parts, and implementing changes can seem intimidating. But with efficient patient throughput playing such a key role in improving the patient experience and reducing the hospital length of stay, it’s one of the most valuable hospital cost reduction strategies available.
Thankfully, with the wealth of digital tools at hand, streamlining throughput in healthcare has become all the more simple and effective. And the sooner you begin to streamline your patient throughput, the sooner your organization will see the benefits.